Links:
- Incidence:
- Incidence of both PF4-Heparin antibodies and HIT are higher in Orthopedic and Cardiac Surgery patients than in General Medicine patients.
- Incidence of PF4-Heparin antibody formation much, much higher than clinical HIT – estimated incidence of antibody formation up to 19% in acutely ill inpatients.
- Incidence higher with UFH than with LMWH use.
- Clinical Features:
- Thrombocytopenia
- Typical onset is 5-10 days after starting UFH
- Rapid onset can occur in <1 day following re-exposure to heparin
- Mild to moderate thrombocytopenia is typical: median platelet count is ~60,000/µL
- Platelet count falls below 20,000/µL in only 15% of cases
- Absolute thrombocytopenia NOT required to consider the diagnosis – an otherwise unexplained drop in platelet count of >50% suggests the development of HIT regardless of total platelet count
- Thrombosis
- Seen in >50% of HIT cases
- Observed irrespective of platelet count nadir
- Thrombosis can even precede platelet decline
- Thromboses can be either venous or arterial, though venous are more common
- Venous locations: DVT > PE >> adrenal vein thrombosis > cerebral sinus thrombosis
- Arterial locations: limb artery > stroke syndrome > MI > mesenteric artery
- Prothrombotic complications if treatment initiated with warfarin:
- warfarin-induced skin necrosis and venous limb gangrene
- Skin lesions at heparin injection sites
- Severity ranges from erythematous plaques to skin necrosis
- Acute systemic reactions following IV heparin boluses
- Acute inflammatory or cardio-respiratory symptoms and abrupt fall in platelet count
- Laboratory Features:
- Absolute or relative thrombocytopenia
- Antigen Assay (Screening Test), aka “:
- Typically EIA platform
- Very sensitive, not very specific
- Often detects clinically insignificant antibodies
- Activation Assay (Confirmation Test)
- Usually Serotonin Release Assay (SRA)
- Highly specific
- Requires specialized laboratory testing, not available in many laboratories (i.e.: will be a “send out”, and have a multi-day wait for a result)
- Pathophysiology:
- HIT antibodies recognize platelet factor 4 (PF4) in complex with heparin
- PF4 antigenic epitopes exposed via conformational changed induced by heparin binding
- Resulting antibodies preferentially bind large multi-molecular complexes of PF4-heparin
- UFH more efficient substrate for complex formation than LMWH
- PF4-heparin-antibody complex bind and crosslink platelet Fc receptors, resulting in platelet activation and release of procoagulant microparticles
- Diagnosis:
- HIT is diagnosed using a combination of clinical and laboratory criteria
- Warkentin’s 4T Scoring System can be used to assess pre-test probability, and better inform use of specific HIT testing (EIA and/or SRA):
- HIT antibodies recognize platelet factor 4 (PF4) in complex with heparin
- Thrombocytopenia
| 4T’s Category | 2 points | 1 point | 0 point |
| Thrombocytopenia | Platelet count fall 50% from baseline and platelet nadir ≥20×109/L | Platelet count fall 30% – 50% from baseline or platelet nadir 10 – 19×109/L | Platelet count fall 30% from baseline or platelet nadir 10×109/L |
| Timing of platelet count fall | Clear onset between days 5 and 10 or platelet fall ≤ 1-day, with heparin exposure within 30 prior days. | Fall in platelet counts consistent with onset between days 5 and 10 but timing is not clear due to missing platelet counts or onset after day 10 of heparin exposure or fall in platelet counts ≤ 1-day with prior heparin exposure (between 30 and 100 days ago). | Platelet count fall within 4 days, without recent heparin exposure. |
| Thrombosis or other sequelae | New thrombosis, skin necrosis, or acute systemic reaction after unfractionated heparin exposure. | Progressive/recurrent thrombosis or unconfirmed but clinically suspected thrombosis. | No thrombosis or thrombosis preceding heparin exposure. |
| Other causes of thrombocytopenia | None apparent. | Possible other causes present. | Probable other causes present. |
- A score of 6-8 indicates a high pre-test probability of HIT, 4-5 intermediate, and 0-3 low probability
- If 4T score is >4, consider EIA (“HIT Antibody”) testing; if ≤3, antibody testing not indicated
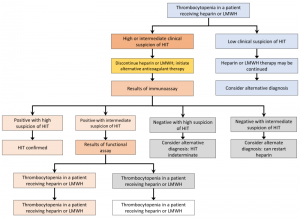
- Many interpretative algorithms available, e.g.:
- Treatment:
- Initiate immediate anticoagulation with an alternative, non-heparin anticoagulant:
- Bivalirudin
- Reversible, direct thrombin inhibitor
- Short half-life (25-30 minutes)
- Dosing for HIT unclear, but suggested initiation at 0.15-0.25 mg/kg/hr and adjusted to PTT of 1.5-2.0 times baseline
- Reduce dose in setting of renal disease/ESRD
- Argatroban
- Small molecule direct thrombin inhibitor
- Treatment of choice for HIT
- Initiate gtt at 2 µg/kg/min, titrate to maintain PTT 1.5-3.0 times baseline (keep less than 100)
- Do not follow PT/INR when on Argatroban – effects highly unpredictable and do not correlate with therapeutic effects
- Reduce dosing for liver disease, heart failure, anasarca
- Transitioning to oral anticoagulation:
- Warfarin
- Should never be initiated until patient is adequately anticoagulated with bivalirudin or argatroban
- Reasonable to wait to initiate until platelet count has normalized
- Warfarin should overlap with IV anticoagulant for at least 5 days, and until INR therapeutic for >48 hours
- Duration of Treatment:
- HIT antibodies are transient – median time to negative EIA (“Heparin Antibody”) is 85 days
- HIT without thrombosis – therapeutic anticoagulation at least until platelet count is normal; some experts suggest continuing anticoagulation for up to 4 weeks
- HIT with thrombosis – therapeutic anticoagulation for at least 3-6 months
- Warfarin
- Bivalirudin
- Initiate immediate anticoagulation with an alternative, non-heparin anticoagulant: