Links:
Protocol:
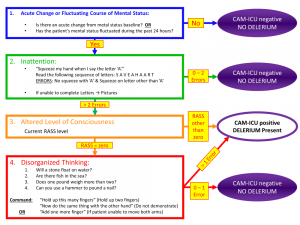
Delerium Protocol (PDF figure)
Delirium can be HYPO or HYPERactive. Both lead to longer and more complicated hospitalizations as well as long-term sequelae. Patients who develop delirium are at risk for having the equivalent of Alzheimer’s or TBI cognitive deficits 1 year out of discharge from an ICU. Be alert for hypoactive delirium
- Initial considerations
- safety – do you need chemical or physical restraints
- look for the underlying cause!
- consider repeating blood cultures, chest X-ray, UA, basic labs, head scanning, LP, EEG
- nonpharm/nonrestraint interventions
- frequent reorientation
- family at the bedside, a sitter (if available)
- lights on during the day (natural light), off at night, minimize nighttime interruptions
- human touch (massage, ideally)
- Minimize deliriogenic meds (anticholinergic meds, benzodiazepines, medications with GABA activity)
- Chemical before physical restraints, discontinue physical restraints ASAP (consider dexmedetiomidine)
- assess – with baseline CAM-ICU and reassess regularly
COMABATIVE/AGITATED/DELIRIOUS PATIENT
- Safety – of patient and staff – number 1 priority
- Is the environment safe? do you need to involve security?
- Goal
- Calm without over-sedating
- Assess for cause of agitation
- secondary to AMS? a PEC they disagree with?
- workup for AMS
- do you need to reassess capacity/involve psychiatry?
- Treatment
- Nonpharm measures – verbal de-escalation
- Chemical before physical restraints – always try PO first
- Restraints
- Assess for discontinuation of restraints often. Close nursing monitoring is required of all restrained patients. 1:1 sitter is required
| Agent | Dose | Half-life | Precautions |
| Dexmedetomidine | 1 mcg/kg over 10 min | 1.8 – 3.1 hr | Bradycardia, loss of airway reflexes, rebound hypertension when discontinued |
| 0.2 – 0.7 mcg/kg/hr | |||
| Haloperidol | 1 – 40 mg IVP | 21 – 24 hr | QTc prolongation, extrapyramidal symptoms |
| Quetipine | 12.5 – 200mg po | 6 – 7 hr | QTc prolongation, extrapyramidal symptoms |
| Olanzapine | 2.5 – 20mg po (there is an orally disintegrating option) | 21 – 54 hr | QTc prolongation and sedation, extrapyramidal symptoms |
| Aripiprazole | 10 – 30mg po | 75 hr | Extrapyramidal symptoms |
| 9.75mg IM |
- Avoid benzodiazepines unless patient is in alcohol or benzodiazepine withdrawal. Benzodiazepines should never be your first choice for a combative patient.
- Different antipsychotics prolong QTc to different degrees: olanzapine < risperidone < quetiapine < haloperidol
- QTc prolongation – most dangerous risk is for Torsades de pointes (2 hit hypothesis – long QT + another risk for arrhythmia = increased risk)
- Discontinue antipsychotics if QTc > 500 or increases by > 25%
- Monitor baseline and 24 hours after initiation of meds
- Be aware of other meds that prolong the QT interval (Zofran, Antibiotics, Antihistamines, Amiodarone, Albuterol, SSRIs)