Links:
The Misunderstood Coagulopathy of Liver Disease: A Review for the Acute Setting
- Coagulopathy in patients with severe liver disease is very complicated, vastly more than “elevated INR = coagulopathic”. Cirrhotics can be hyper- or hypocoaguable!
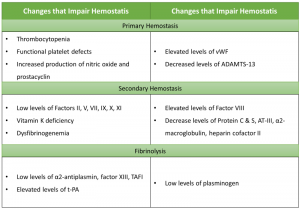
Alterations in Hemostasis in Liver Disease
(from Lisman and Porte, Blood 2010;116:878-885)
- In addition to transfusion support, including management of major hemorrhage as outlined in Massive Transfusion, consider the following points:
- Correction of coagulopathy (if indeed one is present) is likely to require more than merely transfusing large quantities of plasma
- Check, and correct deficiencies in, fibrinogen levels early!
- Fibrinogen should be measured as frequently as CBC, PT/PTT in hemorrhagic patient with liver disease
- Some experts (including editor of this section) suggest transfusing cryoprecipitate for fibrinogen goal of >200 mg/dL in setting of major hemorrhage
- May also consider cryoprecipitate transfusion if dysfibrinogenemia is suspected, irrespective of measured fibrinogen levels (may require discussion with Blood Bank medical director)
- Adjunctive therapies:
- Vitamin K: 5-10 mg IV over 30-60 minutes
- ddAVP: 0.3 µg/kg IV q12h x 1-2 days
- Antifibrinolytic therapies – tranexamic acid (PO: 1-1.5g q6-8h; IV: 1g bolus, 1g IV gtt per 8 hours) or aminocaproic acid (Amicar; 4-12 g/day PO/IV)
- Due to complexity of coagulopathy and potential for complications (including thrombosis), if viscoelastic testing (“TEG” or “ROTEM”) is available at your institution, would strongly suggest sending TEG (thromboelastrography) or ROTEM (thromboelastometry) assays
- TEG is available at UMCNO, Tulane, and SLVHCS
- Results typically available in ~1 hour
- Performed in Blood Bank
- Suggest consultation with Coagulation Attending on Call
- TEG is available at UMCNO, Tulane, and SLVHCS