Pathophysiology: Extensive tumor lysis leads to the rapid release of intracellular contents of dying cells with resultant hyperkalemia, hyperphosphatemia and hypocalcemia. Catabolism of nucleic acids leads to hyperuricemia and AKI secondary to uric acid precipitation in tubules, calcium-phosphate precipitation and xanthinuria.
Diagnosis: Cairo-Bishop classification
| Laboratory TLS | Clinical TLS |
| Uric acid ≥ 8.0 mg/dL | AKI (Cr > 1.5 x upper limit of normal for patient age and sex) |
| Potassium ≥ 6.0 mEq/dL | Cardiac arrhythmia |
| Phosphorus ≥ 4.6 mg/dL | Seizure, tetany, or other symptomatic hypocalcemia |
| Calcium ≤ 7.0 mg/dL | |
| More than 2 out of 4 lab criteria in the same 24-hour period within 3 days before and 7 days after chemotherapy initiation |
Risk Factors for TLS:
| Tumor Related | Clinical |
| High tumor cell proliferation rate | Pretreatment hyperuricemia (serum uric acid >7.5 mg/dL) or hyperphosphatemia |
| Chemosensitivity of the malignancy | AKI or CKD |
| High tumor burden | Oliguria and/or acidic urine |
| Elevated pretreatment serum lactate dehydrogenase greater than twice the upper limit of normal | Dehydration, volume depletion, or inadequate hydration during treatment |
| Increased age | Concomitant use of drugs that increase uric acid |
| Bone marrow involvement |
| RISK OF TLS IN MALIGNANCY | |
| Malignancy | Risk |
| Solid tumors* | Low |
| Multiple myeloma | Low |
| Chronic lymphocytic leukemia ŧ | Low |
| Chronic myeloid leukemia | Low |
| Burkitt lymphoma | High |
| Acute lymphoblastic lymphoma WBC<100,000/mm3(LDH<2X ULN) WBC<100,000/mm3(LDH>=2X ULN) WBC>100,000/mm3 | Intermediate High High |
| Acute myeloid leukemia WBC <25,000/mm3 (LDH<2X ULN) WBC <25,000/mm3 (LDH>=2X ULN) WBC 25,000-75,000/mm3 WBC >75,000/mm3 | Low Intermediate Intermediate High |
*Some solid tumors such as bulky small cell carcinoma are Intermediate/High risk for spontaneous TLS or TLS post treatment
ŧCLL with WBC > 50,000 at initiation of treatment with ibrutinib is associated with intermediate/high risk for TLS
Prophylaxis:
- Volume Expansion – Target fluid intake of 2-3 L/day with IV or oral therapy before start of chemotherapy to maintain glomerular filtration. Urine output goal is >2 mL/kg/hr. Loop diuretics can be used if patients develop volume overload.
- Avoid urine alkalization- this worsens calcium and phosphate deposition even though it increases uric acid excretion.
- Hypouricemic agents
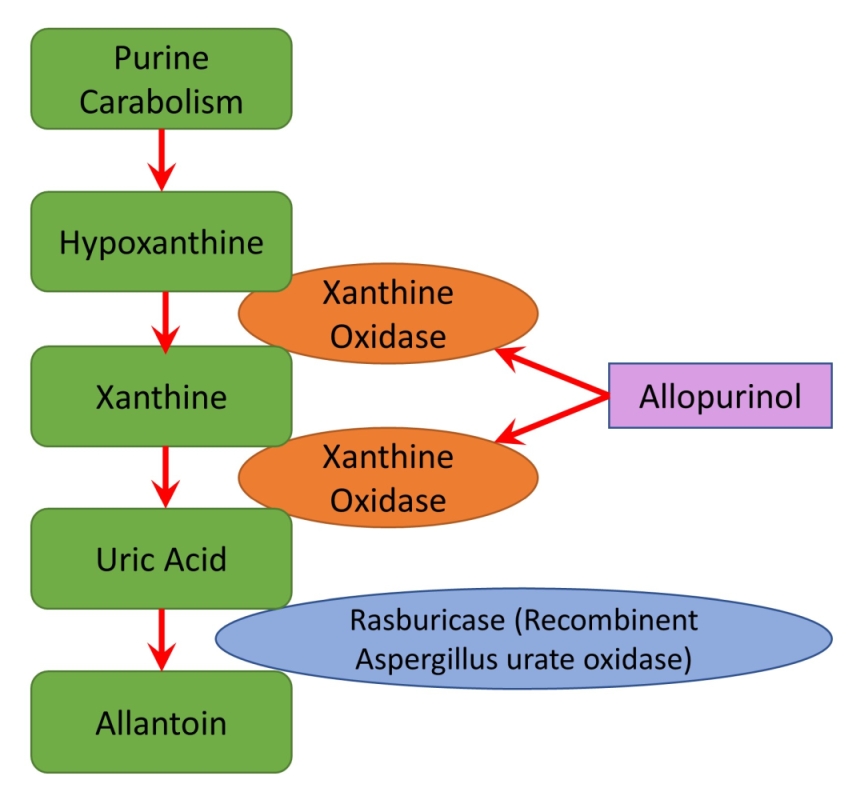
- Allopurinol – Inhibits purine metabolism and increases xanthine and hypoxanthine. It decreases uric acid production but has no effect on existing uric acid levels. The increase in hypoxanthine and xanthine may lead to xanthinuria, deposition of xanthine crystals in the renal tubules, and AKI.
- Rasburicase – Recombinant Aspergillus urate oxidase that converts uric acid to allantoin. It is contraindicated in G6PD deficiency.
TLS Prophylaxis Recommendations
| TLS RISK | Monitoring | Volume Expansion | Allopurinol | Rasburicase |
| Low | X (daily) | X | X | |
| Medium | X (labs q8-12 hrs) | X | X | +/- |
| High | X (labs q6-8 hrs and cardiac monitoring) | X | X | X |
Treatment of confirmed TLS:
- All patients with confirmed tumor lysis syndrome should be admitted to ICU.
- Supportive care – Continuous cardiac monitoring, Monitor electrolytes, Cr, Uric acid Q4 – 6hrs, dietary K and phos restriction
- Rasburicase – Indicated if Uric acid > 8
- Renal replacement therapy indications (requires HD catheter and coordination with Nephrology)
- Severe oliguria or anuria
- Persistent rebound hyperkalemia or hyperphosphatemia
- Hyperphosphatemia-induced symptomatic hypocalcemia
- A calcium-phosphate product ≥ 70
